Golden Standard in the Diagnosis of Rhinitis

A Few Words on the Nose
Like hardly any other organ, the nose has evolved throughout history, and its specific shape has been a symbol of beauty, nobility and sometimes an element of satirical derision. In the popular padawan 'following the Czarnoleski exemplar’, Jan Kochanowski noted the qualities of beautiful women using specific expressions describing the timeless nature of their beauty, such as '...the nose as a rope plaited'. It has also been thought that the very structure of the nose is indicative of the owner's character type. Moreover, the shape of the nose has determined one's position in the world of war strategists. According to philosophers, and following Pascal's aphorism ‘Cleopatra's nose, had it been shorter, the whole face of the world would have been changed', it is widely believed that the right decisions taken are a guarantee of geopolitical stability, while the wrong ones affect the fate of the world. However, back to the substance. The nose recognises nearly 50 000 000 different odours and undertakes the essential functions of thermoregulation, humidification and purification. What's more, we have fourteen types of noses, and one in four of them is similar to Albert Einstein's nose. It is also known that the length of the nasal cavity varies with the age and sex of the subjects: in boys over 16 years of age, a significant increase in CSA-1 (cross-sectional area of the nasal cavity at its valve, measured by acoustic rhinometry) is observed, while in women over 18 years of age, a greater cross-sectional area is observed at a depth of three centimetres behind the nasal valve.
Allergic Rhinitis - a Problem Faced by Many Poles
Within the course of various diseases, the nose plays a key role in the complex pathomechanisms of the allergic reaction, in which common environmental allergens are the main determinants. According to a study carried out by the ECAP project - Epidemiology of Allergic Diseases in Poland, conducted at the Department of Environmental Hazards Prevention, Allergology and Immunology of the Medical University of Warsaw, nearly 40% of the Poles are allergic, and 25% of them are diagnosed with allergic rhinitis. It is a disease entity with an IgE-dependent reaction that may co-exist in the course of other conditions, e.g. with conjunctivitis or asthma. It has the nature of atopy. An interesting and somewhat different form of allergic rhinitis is local allergic rhinitis. It is treated as an isolated response within the nasal mucosa. The causes are the same as in allergic rhinitis. It should be mentioned that the specific carrier for the allergen is air pollutants, the so-called adjuvants of the inflammatory response, which are a common problem on a global scale. Local allergic rhinitis is identified, with nearly 25% of patients diagnosed with rhinitis. The patient profile is even defined: she is a 32-year-old woman living in a large urban area, a non-smoker and allergic to house dust mite allergens, birch and grass pollen. Her clinical history revealed a family history of allergic diseases. The diagnostic difficulty in differentiating this type of condition in the rhinitis group is that it has a localised reaction and therefore, with a clinical history confirming allergy, skin tests and serum sIgE are negative.
Intranasal Allergen Challenge Test Is a Good Alternative for the Diagnosis of Rhinitis
The only recommended method for the diagnosis of local allergic rhinitis is the intranasal allergen challenge test. It is also an relevant element in the differential diagnosis of allergic rhinitis, in which the reaction is systemic. The observed reaction in the intranasal challenge test is immediate. It is sometimes referred to as a ‘local anaphylactic reaction within the nasal mucosa’, in which the allergen is presented (by the APC presenting system) to Th2 lymphocytes. As a result, there is a release of: IL-4 and IL-13, which in turn stimulate B lymphocytes to produce IgE and cytokines. These, in turn, mobilise the eosinophil cell for specific migration in the submucosal layer and the mucosa itself. As a consequence of the complex reactions, the allergen combines with sIgE to coat the mast cell in the effector tissue. This contributes to the release of preformed mediators, which include, inter alia, tryptase. In parallel, there is a synthesis of mediators that are secreted by the mast cells (platelet-activating factor, PAF, formed from arachidonic acid, LTC4, LTD4, PGD2, PGI2 and substance P). The secondary effect of these complex processes is the early phase (occurring within the first 60 minutes after contact with the allergen) and the late phase of the allergic reaction (4 - 48 hours after local application of the allergen).
Typical symptoms of the early phase are nasal pruritus, sneezing, an increase in serous discharge and nasal cavity obstruction observed at 10-20 minutes of examination. Symptoms persist for about an hour and smoothly progress to the late phase, in which stimulated cells release cytokines and chemokines into the blood, resulting in the ejection from the bone marrow of leukocytes: eosinophils and their precursors. Inflammatory cell infiltration in the nasal mucosa is observed, which results from the influx of eosinophils and the proliferation of precursor cells. There is a potential risk of dyspnoea and cough during this phase of the study, especially in patients who are diagnosed with asthma. A good option in this case is to assess the functional status of the lower airways performed by spirometry (percentage decrease in FEV1) and/or nitric oxide levels in exhaled air.
Standardisation of Nasal Patency Assessment Tools in the Spotlight of Interest of Researchers from the MUW
As it has already been mentioned, under controlled outpatient conditions and using standardised tools to assess nasal patency (including functional: rhinomanometry and peak nasal inspiratory flow - PNIF, and structural: acoustic rhinometry), the intranasal allergen challenge test mimics the natural response of the nasal cavity mucosa to the applied allergen. This is a particular area of interest for our team, which is one of the few leading centres in the country and abroad working on the standardisation of the aforementioned techniques of objective nasal patency testing.
A rhinomanometer is a device equipped with a mask and a pneumotachograph connected to a head that is compatible with a specially adapted computer. Its principle of operation is based on the determination of the resistance of air flowing through the nasal cavity. This makes it possible to measure the volume of air and assess the pressure difference between the front and back nostrils, which are responsible for this flow. Intranasal resistance is measured at a flow rate of 100-150 ml/s or a pressure difference of 0.10-0.15 kPa. The measured flows are laminar, turbulent and mixed, respectively. The inhaled air, after passing through the first nasal segment - the anterior nostrils - changes direction from vertical to horizontal. As it changes, there is a corresponding increase in the flow of air in a given unit of time. The variation in flows is dictated by the anatomical structure of the nasal cavity: in its first section at the level of the nasal vestibule and near the head of the inferior nasal auricle.
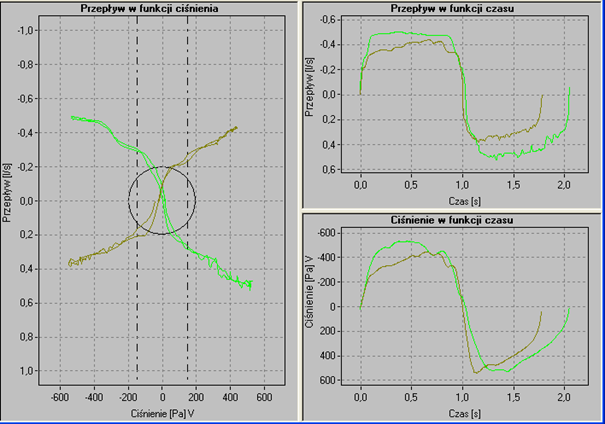
The secondary effect of flow variation (Y-axis) relative to measured pressure (X-axis) is shown in Figure 1 illustrating precisely the functional nasal patency .
A second important tool for assessing objective nasal patency is the PNIF, which is the inverse of peak expiratory flow PEF and is dependent on the level of cooperation of the subject. The result is the average of three correctly performed, repeatable measurements. In an attempt to search for reference values for this testing technique, we conducted a study on a group of 4,137 subjects, which shows that the final measurement result is not only influenced by the technique, but also by the sex and age of the subjects. Higher nasal inspiratory flow assessment parameters was presented by men of working age vs. female subjects.
Acoustic rhinometry deserves special attention in the group of techniques that structurally objectivise the intranasal spaces. Its principle is based on the reflection of an acoustic wave (generated by a sound generator connected to a tube that transmits the acoustic wave into the nasal cavity and back via a transducer to a computer) from the intranasal spaces.
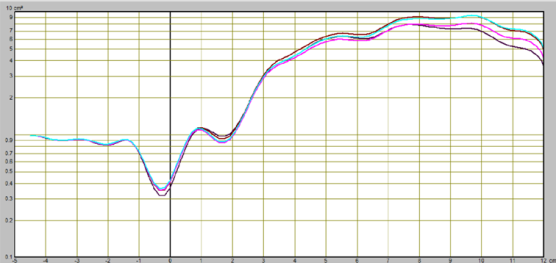
Dzięki temu kreśli się krzywa przekrojów poprzecznych jamy nosa: na osi X obrazuje głębokość jamy nosa, natomiast na osi Y – powierzchnię przekroju poprzecznego.
As a result, a cross-sectional curve of the nasal cavity is drawn: on the X axis, it shows the depth of the nasal cavity, while on the Y axis, it shows the cross-sectional area. The essence of interpreting the test result is to delineate on the rhinometric curve the areas under study: the nasal passages and the head of the inferior nasal auricle. The individual points on the arm of the curve correspond respectively to: 0 - the beginning of the nasal cavity, I (Isthmus nasi) - the peak point of the first slope of the rhynometric curve, corresponding to the first constriction of the nasal cavity, C (Concha nasalis)- the peak point of the constriction of the second slope of the rhynometric curve, corresponding to the second constriction of the nasal cavity, E - the distal segment of the head of the inferior nasal auricle, F - the highest point on the rise of the rhynometric curve between points I and C. The areas in these points describe the spaces: 0 - I - nasal vestibule, I - C - distance between the nasal isthmus and the head of the inferior nasal auricle, C - E - end of the nasal auricle, E - G - nasopharyngeal space. Nasal patency disorders (in the course of an intranasal challenge test, in a positioning study in obstructive sleep apnoea, or in an ischaemia of the nasal cavity mucosa) are defined in three relevant areas: maximal nasal cavity constriction (MCA - Minimal cross sectional area: MCA1, MCA2); decreases/increases in nasal cavity volume (V1, V2) and cross sectional area of the nasal cavity CSA (Cross sectional area), which correspond successively to point I (Isthmus nasi) and C (Concha nasalis) on the arm of the rhinometric curve (CSA-1, CSA2). While experts from The European Academy of Allergy and Clinical Immunology in the EAACI Position paper on the standardisation of nasal allergen challenges indicate the particular usefulness of these three, the American researchers draw attention to another important technique for assessing patency in the course of an intranasal allergen challenge test. This is an analyser of nitric oxide levels in the air exhaled from the upper airways. Nitric oxide is formed by enzymes from the nitric oxide synthase group and plays a physiological role in the upper airways by maintaining, among other things, the sterility of the paranasal sinuses. In the course of inflammatory conditions, including allergic rhinitis, it reaches high values measured in thousands (ppB) relative to the physiological state. In the challenge test, nitric oxide shows a decreasing trend in the early phase of the allergic reaction. In contrast, a significantly higher level is observed in the late phase relative to the baseline value. This variation should be explained by the obstruction of the paranasal sinus outlet as a consequence of the intranasal challenge test with the allergen in the early phase of the allergic reaction and the release of this marker of the inflammatory response in the late phase of the allergic reaction, in which the swelling is relieved.
The criteria for the so-called remarkably and moderately positive allergen challenge tests were developed for all previously described techniques. In the procedural technique group, a decrease in flow of 40% or more is an expression of a remarkably positive challenge test. In contrast, a moderately positive challenge test is considered to be one in which the flow decreases to a level of 20% relative to the condition before the application of local allergen. In the acoustic rhinometry, on the other hand, a decrease of 40 % in CSA-2 transepithelial cross-sectional area is indicative of an extremely and 20 % of a moderately positive challenge test. In our study, in an attempt to assess the degree of response of the nasal mucosa to the applied allergen as measured by the nitric oxide level in the exhaled air, we estimated a 37% decrease in this inflammatory response marker as an expression of a positive challenge test.
When making an attempt to find other alternative techniques for assessing nasal patency applicable to the intranasal allergen challenge test, we used optical rhinometry. This innovative device, called an emission spectrometer, has a detector and a transmitter placed on opposite sides of the nose. It emits a beam of infrared light with an average wavelength of 600-800 µm at a frequency of 0.2 seconds. In this manner, it accurately determines the beginning (T1), maximum intensity (OD - optical density) and end of the allergic reaction (T2).
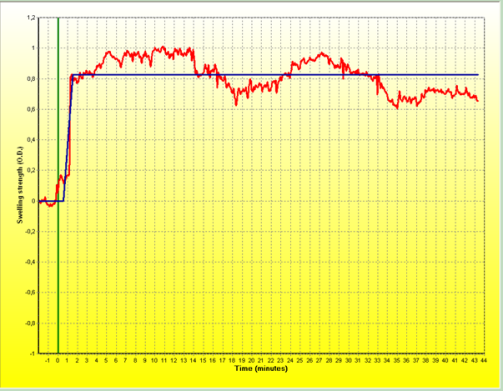
The principle of operation of the device is similar to pulse oximetry. In our observations, the beginning of the reaction measured by optical rhinometry in the intranasal challenge test occurred in the 2nd minute of the test (upon a local application) and its highest intensity (swelling of the nasal cavity mucosa) was recorded in the 10th minute and amounted to 0.4552 OD.
Intranasal Challenge Test and Diagnosis of Food Allergy
Facing the recommendations of The European Academy of Allergy and Clinical Immunology contained in the EAACI Position paper on the standardisation of nasal allergen challenges in the field area of broadening the indications for the challenge test, more and more attention is being paid to the cognitive potential of this test in diagnosing food allergy. The first study was conducted by American researchers and consisted of observing the response of the nasal mucosa to a food challenge (with placebo). For this purpose, vision thermography was used, which demonstrated a significantly substantial increase in temperature in the nasal cavity area during the early phase of the allergic reaction. Two years later, the same researchers performed an intranasal challenge test with peanut allergens (allergen extract 10 μg suspended in 100 μl physiological saline), which proved to be a milestone in this area of diagnosis. A full picture of the immediate response in the nasal mucosa was observed as early as at 18.20 minutes of the test: nasal pruritus, leakage of watery discharge, and nasal cavity obstruction. The complaints persisted over the next 60 minutes. It should be noted that no complications were observed, including an anaphylactic reaction to the intranasally administered allergen. The development of the form and dose of the allergen is of critical importance for the standardisation of the intranasal challenge test with food allergens. The Spanish researchers met this challenge by developing a lyophilised extract of cooked shrimp mixture using the Bradford technique under the laboratory conditions. In a precisely designed study, the lyophilizate dissolved in physiological saline was administered intranasally in successively increasing doses of 1:100, then 1:10 and, in the final stage of the study, 1:1. Out of 21 subjects, 18 patients allergic to shrimps had a positive outcome of the intranasal challenge test (specificity 90%, sensitivity 89%). The only symptoms observed in the so-called non-nasal group were itching of the throat and palate. This undoubted scientific success initiated, also in our research centre, work on the standardisation of the method and its application for food allergy diagnosis.
The intranasal allergen challenge test can also be performed under stationary conditions, e.g. using the Vienna Chamber, or under laboratory conditions using the basophil activation test - BAT, the so-called challenge test in a test tube. In parallel to the assessment of the degree of nasal mucosal oedema measured by the objective techniques discussed, the subjective complaints of the patient are assessed, e.g. using the Visual Analogue Scale, VAS or Total Nasal Score. The sum of the subjective (VAS > 55mm or Total Nasal Score > 5 points) and objective assessments defines the degree of response to the applied allergen.
I would like to cordially invite you to read and explore the issues
in the field area of differential diagnosis applicable to rhino- and allergology.
References at the author's address.
Edited by: Communication and Promotion Office
Photos: Tomasz Świętoniowski, Marcin Szumowski; Communication and Promotion Office