Interventional radiology is a field of medicine in which doctors perform therapeutic and diagnostic procedures under the guidance of imaging tests such as X-rays, computed tomography, magnetic resonance imaging, or ultrasound. A part of this field is interventional oncology, that is, interventional radiology in oncology—a specialty dealing with minimally invasive treatment of patients with cancer.
Interventional radiology is present at every stage of cancer - says Grzegorz Rosiak, MD, PhD, Vice-Chairman of the Treatment Section of the Polish Medical Radiological Society UCK WUM. This field covers many procedures: minimally invasive diagnostics (biopsies), therapeutic procedures (thermoablation, cryoablation, chemoembolization, and radioembolization), pain management (neurolysis, blockades, cryoneurolysis), and finally, treatment of complications following other oncological therapies (e.g., abscess drainage, embolization of bleeding). As a result of these procedures, many patients can avoid major surgery, and the recovery time is significantly shorter.
Biopsy – the foundation of modern diagnostics
In the era of personalized medicine, oncological diagnostics require the collection of an adequate quantity and quality of material for histopathological and molecular testing.
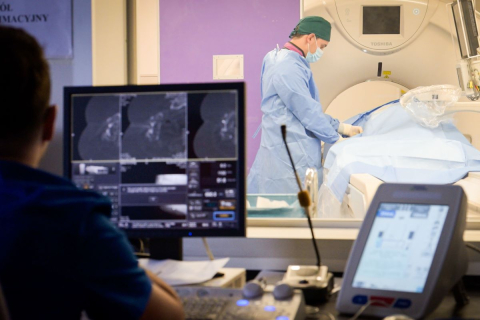
Interventional radiologists perform CT-guided core needle biopsies, which allow for the precise collection of material from tumors in the liver, lungs, kidneys, pancreas, lymph nodes, or bones.
This approach enables a fast and reliable diagnosis as well as the selection of targeted therapy. Unfortunately, in Poland, fine-needle biopsies are still used too often – they do not provide a sufficient amount of diagnostic material and often need to be repeated.
Thermoablation and cryoablation – precise destruction of tumors
Thermoablation and cryoablation procedures enable the destruction of tumors without surgical intervention.
Through a thin needle inserted through the skin into the tumor, the doctor delivers heat or cold energy that destroys cancer cells. The procedure takes several dozen minutes, and the patient usually returns home after 1–2 days.
These methods are used in the treatment of liver, lung, kidney, and bone tumors, and have been included in international oncology guidelines for over 20 years.
Chemoembolization and radioembolization
Under angiographic guidance, the physician inserts a catheter into the blood vessel supplying the tumor and administers the drug or radioactive material directly to the tumor, limiting toxicity to healthy tissues.
These procedures are particularly effective in treating liver tumors—in many cases, they are a safer and more effective alternative to conventional chemotherapy.
Treatment of pain and complications
Interventional radiologists also perform pain-relieving procedures, including neurolysis and cryoneurolysis, as well as life-saving procedures such as abscess drainage and embolization of bleeding vessels. As a result of these procedures, repeat surgeries can be avoided and hospitalization time can be significantly reduced.
Access to radiology procedure
Interventional radiology in oncology (interventional oncology) is one of the most dynamically developing fields of modern medicine. In Western countries, it is one of the four basic pillars of oncological treatment (clinical oncology, oncological surgery, radiotherapy, interventional radiology).
Unfortunately, according to estimates by the Polish Medical Radiological Society, as many as 90% of Polish oncology patients currently do not have access to interventional radiology procedures - says Grzegorz Rosiak, MD, PhD. Many minimally invasive treatment methods that offer a real chance of recovery in other countries are still not used in Poland. Instead, older, often palliative therapeutic methods dominate – less effective for the patient and significantly more expensive. Meanwhile, interventional radiology reduces the costs of therapy, reduces the number of complications, shortens the length of hospitalisation and reduces the need for outpatient visits, while delivering better treatment results.
Introduction of reimbursement
However, in January 2025, a huge step forward was taken – the Ministry of Health introduced reimbursement for thermoablation and cryoablation of lung, bone, and adrenal tumors. This is a groundbreaking decision that paves the way for broader use of these modern, minimally invasive cancer treatment methods. Unfortunately, most centers lack the appropriate equipment, which means that even reimbursed procedures cannot be performed.
As part of the National Oncology Strategy (NSO), investment support for interventional radiology has been planned. Task 23.5 states: “Between 2023 and 2026, we will finance investments in equipment and medical devices intended for performing interventional radiology procedures, with the aim of ensuring that oncology patients receive a therapeutic process of appropriate quality and safety.”
Unfortunately, although approximately PLN 1.5 billion has so far been allocated for investments in medical equipment within the NSO budget, no funds have been allocated to interventional radiology - says Dr. Rosiak. We hope that in 2026, NSO budget funds will finally be allocated to investments in equipment and facilities for interventional radiology laboratories, so that by implementing the Strategy’s goals, the availability of minimally invasive treatment methods will improve, thereby reducing costs for the payer.
From the patient's perspective
Patients have already experienced the benefits of interventional radiology. Ms. Bożena, a patient from Gdynia:
I am convinced that interventional radiology saved my life. I have been battling cancer for eight years now. In 2024, a team of interventional radiologists led by Grzegorz Rosiak, MD, PhD, performed two thermoablation procedures on my secondary lung tumors (sarcomas). The first procedure was particularly important, as it targeted an aggressive tumor in my left lung that could not be destroyed by other methods. Due to the minimally invasive nature of the procedures, they are incredibly gentle on the patient. I am aware of this because I had previously undergone two traditional surgical tumor removal procedures. Unfortunately, after these procedures, another metastasis appeared in the sacrum. Radiotherapy was applied, but it was ineffective – the lesion continued to grow. Since it was not possible to perform the ablation of this lesion in Poland, it was carried out in France. In the latest check-up, the tumor had practically disappeared – the effect is therefore phenomenal. Without interventional radiology, such effective treatment would not have been possible.
International Interventional Oncology Awareness Week runs from October 27 to 31 this year.