The procedure was performed on July 8 on a 14-year-old patient. The adolescent had already undergone several therapeutic endoscopic procedures and surgical treatment for esophageal achalasia, combined with an anti-reflux operation. He also experienced a recurrence of symptoms in the form of difficulty swallowing.
What is esophageal achalasia?
Achalasia is a disease that causes swallowing disorders due to the lack of relaxation of the lower esophageal sphincter and the absence of esophageal peristalsis. As a result, swallowed food remains in the esophagus and does not reach the stomach.
Surgical treatment of achalasia
Surgical treatment of achalasia involves performing a myotomy, which is an incision of the lower esophageal sphincter, allowing swallowed food to reach the stomach. Simultaneously, a fundoplication, an anti-reflux procedure, is performed to prevent the backflow of stomach contents into the esophagus.
Planimetry and what it involves
In patients after surgical treatment of esophageal achalasia, it is difficult to assess by conventional methods whether the recurrence of symptoms results from the underlying disease (achalasia) or from the fundoplication procedure (an anti-reflux procedure).
This is where esophageal impedance planimetry comes in. The procedure measures the compliance of the esophageal wall (in the area of the lower esophageal sphincter) to stretching and evaluates esophageal motility. It can be performed under general anesthesia. This is particularly important for children, for whom traditional esophageal manometry may be impossible due to lack of cooperation.
When the new procedure may be applied
Impedance planimetry can be performed for a range of indications, such as motility disorders or esophageal narrowing. It enables diagnosis when conventional methods fail. It can also be used intraoperatively to assess the effectiveness of esophageal surgery (for myotomy, fundoplication, etc.), significantly improving therapy outcomes. It may also serve as a standalone therapeutic procedure for treating esophageal strictures.
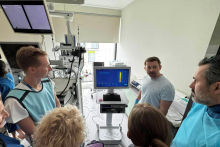
Efforts to bring the equipment needed for planimetry to Poland have been ongoing for several years, and now they have succeeded. The pioneering procedure was performed for the first time in Poland by a team consisting of Dr. hab. Marcin Banasiuk, Dr. hab. Marcin Dziekiewicz, nurse Beata Winnicka, and anesthesiologist Dr. Paulina Trojanek.